Vagus nerve stimulation devices can support mental health for many individuals, managing stress, anxiety, or depression, offering a promising future for mental health management.
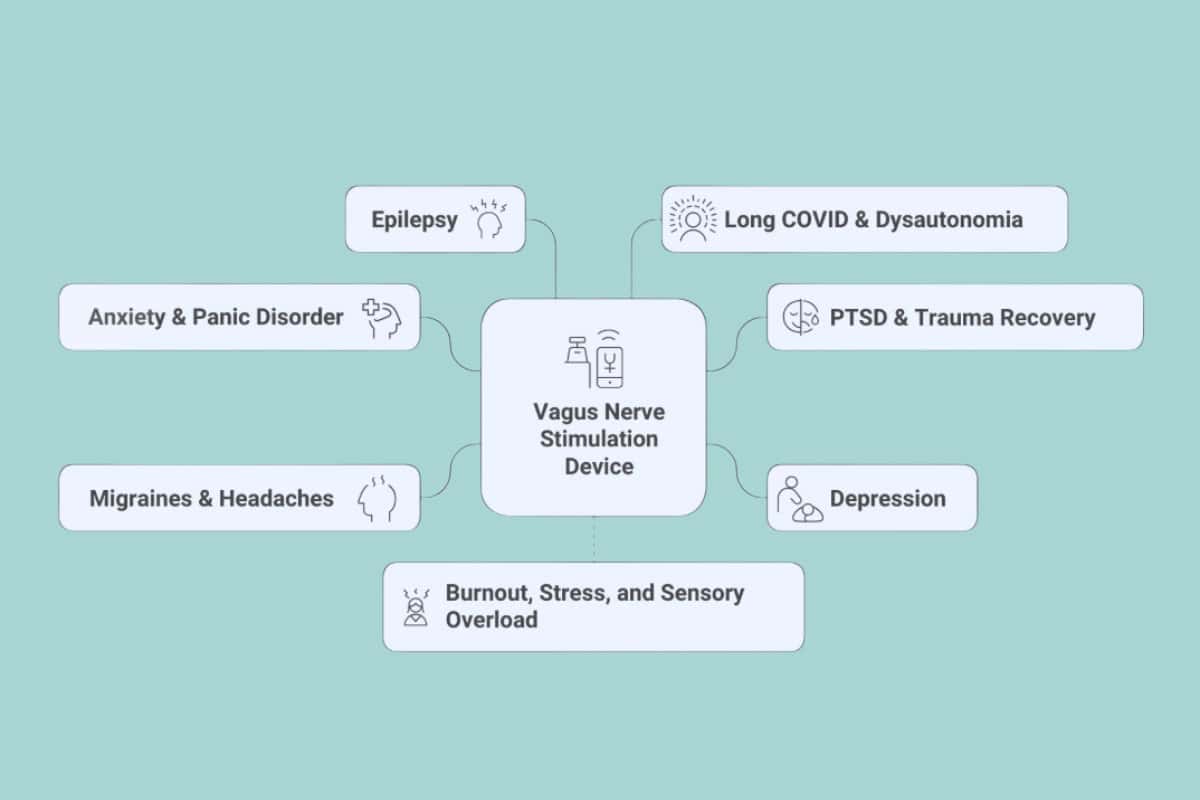
For many individuals, managing stress, anxiety, or depression can be a daunting challenge, even after attempting therapy or medication. However, there is hope in the form of VNS devices. These innovative technologies, which utilize mild electrical pulses to modulate the body’s natural stress and mood systems, provide a new avenue for relief, offering a promising future for mental health management.
Vagus nerve stimulation devices play a crucial role in supporting mental health by helping balance the nervous system and reducing the body’s stress response. This reassures individuals that the technology is designed to effectively manage their mental health.
The vagus nerve connects the brain to major organs and helps control mood, heart rate, and inflammation. By stimulating it, these devices may calm overactive stress pathways and support emotional stability.
Research has shown that both implanted and noninvasive VNS devices can significantly improve symptoms of depression, anxiety, and post-traumatic stress disorder. This promising data should encourage individuals to consider VNS as a viable treatment option for their mental health conditions.
As interest in non-drug treatments grows, VNS devices offer a practical way to target the mind-body connection. Understanding how they work, their potential benefits, and their safety can help individuals determine if this approach aligns with their mental health goals.
How Vagus Nerve Stimulation Devices Work for Mental Health
Vagus nerve stimulation influences how the brain and body respond to stress, emotion, and inflammation. It uses mild electrical impulses to adjust nerve activity that connects the brain to major organs, which may help regulate mood and emotional balance.
Role of the Vagus Nerve in Mood and Emotional Regulation
A vagus nerve stimulation device serves as a vital connection between the brain and the heart, lungs, and digestive system. It not only controls heart rate, breathing, and digestion but also plays a significant role in emotional regulation, a fascinating aspect of our body's intricate system.
This nerve acts as a communication bridge between the body and the brain. It sends signals that influence how a person responds to stress and recovers from emotional distress.
Low vagal activity often relates to anxiety, depression, and poor stress control. Vagal tone—the body's ability to shift from a state of stress to one of calm —is a key factor in emotional regulation. By increasing vagal tone, people may experience calmer moods and better emotional control. Deep breathing, meditation, and the use of a vagus nerve stimulation device can help activate this nerve safely and noninvasively.
Mechanisms of Vagus Nerve Stimulation in the Brain
Electrical impulses from vagus nerve stimulation travel through the nerve to brain regions that control mood and stress responses. These include the amygdala, hippocampus, and prefrontal cortex.
The stimulation helps balance activity between the sympathetic and parasympathetic systems. This balance reduces the body’s “fight or flight” response and promotes relaxation.
Research also indicate that stimulation can impact the hypothalamic–pituitary–adrenal (HPA) axis, which regulates cortisol levels. Lower cortisol levels often mean less anxiety and better mood stability. This mechanism explains why VNS may benefit conditions such as depression and post-traumatic stress disorder.
Types of Vagus Nerve Stimulation Devices
There are two main types of vagus nerve stimulation devices: implantable and noninvasive.
1. Implantable devices require minor surgery to place a small pulse generator under the skin of the chest. Wires connect this generator to the vagus nerve in the neck. It sends timed electrical pulses automatically.
2. Noninvasive devices use external electrodes placed on the neck or ear. They deliver mild electrical signals without the need for surgery. These devices are easier to use and more affordable for many people. Both types aim to regulate nerve activity and support better mental health outcomes.
Impact on Neurotransmitters and Brain Regions
Vagus nerve stimulation influences several neurotransmitters that affect mood, such as serotonin, norepinephrine, and gamma-aminobutyric acid (GABA). Adjusting these chemicals can help reduce symptoms of depression and anxiety.
It also affects brain regions involved in emotional control. The prefrontal cortex becomes more active, which supports better decision-making and emotional awareness.
At the same time, activity in the amygdala, which triggers fear and stress responses, may decrease. This balance between calm and alertness helps explain why consistent stimulation can lead to more stable emotional states.
Mental Health Benefits, Applications, and Safety of Vagus Nerve Stimulation
Vagus nerve stimulation (VNS) devices can help manage several mental health conditions by influencing brain areas that control mood, stress, and inflammation. Research shows that both implanted and external VNS methods can improve symptoms in people with depression, anxiety, and post-traumatic stress disorder (PTSD).
Treatment-Resistant Depression and Mood Disorders
VNS has gained attention as a therapy for treatment-resistant depression (TRD), where standard antidepressants and psychotherapy have not worked. The device sends mild electrical pulses to the vagus nerve, which connects the brain to many organs and helps regulate mood.
Clinical studies show that implanted VNS can improve mood and energy levels over time. Some patients with major depressive disorder or bipolar disorder experience fewer depressive episodes and better emotional stability.
VNS may influence neurotransmitters such as serotonin and norepinephrine, which play key roles in depression treatment. It can also improve vagal tone, the body’s ability to transition from a state of stress to one of calm. Compared to electroconvulsive therapy (ECT), VNS is less intense and does not require anesthesia, though it may take longer to show results.
Reducing Anxiety and PTSD Symptoms
Stimulating the vagus nerve can calm the body’s stress response and lower cortisol levels. This shift from the 'fight-or-flight' response, the body's natural reaction to stress that prepares it to either fight or flee, to the 'rest-and-digest' response, which conserves energy and promotes digestion, helps reduce anxiety and symptoms of PTSD.
People with PTSD often have overactive stress circuits in the brain. VNS can help balance these circuits by affecting areas such as the amygdala and prefrontal cortex. Some studies report significant improvements in emotional control, sleep, and concentration, providing reassurance and confidence in the potential of VNS.
Noninvasive VNS has also shown promise for lowering heart rate and blood pressure during stress. These effects may support long-term emotional resilience and recovery from trauma-related symptoms.
Invasive vs. Noninvasive Vagus Nerve Stimulation
Invasive VNS involves a minor surgical procedure to implant a device under the skin near the collarbone, with a wire connecting it to the vagus nerve in the neck. This method has FDA approval for epilepsy and treatment-resistant depression, offering a more permanent solution.
Noninvasive VNS (such as transcutaneous vagus nerve stimulation, or tVNS) works through external devices placed on the ear or neck. It delivers electrical impulses without the need for surgery, making it easier and less costly to use.
Both forms target similar nerve pathways but differ in intensity and convenience. Noninvasive options, such as transcutaneous vagus nerve stimulation (tVNS), may suit people who prefer a less medical approach or want to combine therapy with lifestyle habits like exercise and meditation. It can also be a suitable option for those who are not eligible for or prefer to avoid surgery.
Potential Side Effects and Safety Considerations
Most users tolerate VNS well, but some experience mild side effects. Common issues include throat pain, changes in voice, coughing, or difficulty swallowing, which can be caused by stimulation near the vocal cords. These effects often fade as the body adapts or device settings change.
In rare cases, surgical VNS can cause infection or discomfort at the implant site. Doctors usually monitor patients closely after implantation to adjust settings and minimize problems.
Noninvasive devices have fewer risks but may still cause temporary tingling or skin irritation. Overall, both forms of VNS appear safe when used under medical supervision and may serve as a valuable addition to standard mental health treatments.
Conclusion
Vagus nerve stimulation devices show promise as tools for balancing the body’s stress and mood systems. They work by sending small electrical pulses to the vagus nerve, which links the brain and body. This process may support emotional regulation and reduce symptoms of depression, anxiety, and PTSD.
Researchers continue to investigate the impact of these devices on brain activity, inflammation, and heart rate patterns. Early results suggest that noninvasive devices could make this therapy more accessible and convenient than surgical implants.
As understanding grows, these devices may become part of a broader approach to mental health care. They can complement therapy and medication, rather than replace them, offering an alternative option for individuals who do not respond well to standard treatments.
This article is for informational purposes only and is not medical advice. Always check with a healthcare professional before using vagus nerve devices, as results and safety can vary.
















Comments
No Comments